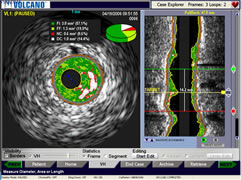
Intravascular
ultrasound images
from console:
cross-sectional (l)
and reconstruction
(r)
courtesy Volcano Corporation |
What
is IVUS?
Intravascular Ultrasound (or IVUS) allows us to see a coronary
artery from the inside-out. This unique point-of-view picture,
generated in real time, yields information that goes beyond what
is possible with routine imaging methods, such as coronary angiography,
performed in the cath lab, or even non-invasive Multislice CT scans.
This cross-section
view can aid in stent sizing, and in confirmation
that the stent has been placed optimally, is fully
expanded and hugging the vessel wall. A growing number
of cardiologists feel that the new information yielded
by IVUS can make a significant difference in how
a patient is treated, and can provide for more accurate
stent placement, reducing complications and the incidence
of stent thrombosis.
How Does IVUS Work?
IVUS uses echocardiography: the same technology as the ultrasound imaging used
in treadmill tests and many other medical exams. Very high frequency sound
waves, called ultrasound, are emitted by a transducer. These ultrasound waves,
which are beyond the range of human hearing, bounce off the various types
of tissue structures in the body and the echo of these waves is then converted
into a picture.
intravascular ultrasound image,
courtesy Volcano Corporation |
In the case of Intravascular
Ultrasound, the transducers have been miniaturized
to less than four hundredths of an inch and placed
on the tip of a catheter. This catheter can be slipped
into the coronary arteries over the same guide wire
that is used to position angioplasty balloons or
stents. It becomes, in effect, a tiny camera that
gives us a cross-sectional view of the artery, a
view that shows distinct circular layers, using shades
of gray or colors, the major ones being:
- the adventitia --
the outer covering of the artery;
- the media --
the actual wall of the artery;
- the intima --
a layer of endothelial and other cells
that make direct contact with the blood inside
the artery
-- in normal arteries this layer is
thin; in diseased
arteries (shown here) the intima is
thickened by plaques or other tissue growth, often
eccentric
or asymmetrical;
- the lumen --
the actual open channel of the artery
through which the blood flows.
How is IVUS Different from Standard Angiography?
The
current “gold standard” of invasive
angiography shows only the lumen, as an X-ray shadow
image created by the injection of contrast dye (as
seen on the left).
Although
angiography shows "narrowings",
as well as a dynamic picture of the blood flow, it
does
not differentiate the other layers (or even the plaque
itself, as shown in the artist's rendition on the right).
In several situations, the increased information
provided by Intravascular Ultrasound literally can change the picture
of the disease, and affect treatment decisions. For example, in a normal
artery the intimal layer is thin -- when measured, there is little difference
between the diameter of the lumen (open channel) and the diameter of
the media (the arterial wall). In a "blocked" or diseased artery,
the intima is thickened by plaques or other tissue growth, and the lumen
diameter is reduced.
But often the plaque or tissue growth is not
evenly distributed, resulting in an eccentric shaped lumen. This eccentric
shape is clearly shown by intravascular ultrasound. But the X-ray angiogram
only shows a "side-view" and the eccentric shape is not seen.
Depending on the angle of view, this may make the artery look more blocked
than it really is -- or conversely, may give a false impression that
the artery is only slightly blocked and does not need to be treated.
With IVUS, just a few clicks on the console measures the area of the
blockage, the size of the artery and yields an accurate percentage of
narrowing.
Another example is that sometimes the plaque
pushes deeper into the vessel wall, giving the appearance that the lumen
is not significantly blocked. Yet a significant amount of diseased plaque
may exist within the arterial wall, ready to rupture and cause a cascade
of events, resulting in a heart attack. This is called vulnerable plaque,
and cannot be visualized using standard angiography.
When is IVUS Done?
Intravascular ultrasound is done in the catheterization laboratory in
conjunction with angiography. Some cardiologists use it occasionally,
in difficult cases, or to assist in the selection and sizing of stents
and balloons. Others use it routinely, to confirm accurate stent placement
and optimal stent deployment.
How Can IVUS Make Stenting More Accurate?
One of the causes of stent thrombosis or restenosis is poor "stent
apposition" -- the stent has not been expanded to the full width
of the artery, and this under-expansion creates a "pocket" which
can collect platelets and other debris, causing a reblockage. Research
conducted using IVUS has confirmed that one of the causes of restenosis
is inadequate dilatation; that is, physicians, concerned with injuring
or dissecting the artery with a balloon inflation, have tended to "play
it safe" and end up under-sizing or under-inflating the balloon
and stent.
With the accurate measurements of both the true
diameter of the artery and the diameter of the open lumen channel provided
by IVUS, the guesswork is taken out of choosing the correct size balloon
and stent. Using only angiography, a cardiologist may underestimate the
size of a diseased artery.
IVUS can also measure the length of the diseased
area, so the precise length of the stent needed can be determined ahead
of time, reducing the need for overlapping stents which are known to
increase the risk of thrombosis.
Once the stent has been implanted, IVUS can
clearly show the stent struts in relation to the arterial wall and plaque.
If the stent has been undersized or if there is any area that needs "touching
up", a larger balloon can be directed to it and expanded to fit
the stent optimally.
Although IVUS was first used over 20 years ago,
the current concerns over stent thrombosis and patient outcomes have
spurred a new interest. The recent S.T.L.L.R.
study, sponsored by Johnson & Johnson, showed that current
DES deployment techniques led to some form of geographic miss in 66.5%
of patients. That means two-thirds of stents are not optimally placed,
which translates into negatively impacted patient outcomes, with significantly
higher restenosis, thrombosis and myocardial infarction rates in patients
where the stent was not placed properly. The study concluded that "a
re-examination of stent placement technique including the use of IVUS
is certainly warranted."
Modern IVUS systems are completely integrated
into the catheterization lab and with proper training, the cardiologist
can add this new imaging technology to a standard diagnostic angiogram
with a minimum of impact on the patient.
 For more information visit our Intravascular Guidance Center. For more information visit our Intravascular Guidance Center.
Revised February 2013, Angioplasty.Org staff |