![]()
<< To Homepage >>
<<Archives>>
May 2009 Archives: May 26, 2009 -- 5:45pm EDT Breaking News -- Texas Senate Passes Calcium
Scoring Bill Late update: Leaders of the Society for Heart Attack Prevention and Eradication (SHAPE) have issued a press release explaining how this legislation will benefit patients and reduce costs. They are urging Texas Governor Rick Perry to sign the bill into law « permalink » « send comment » « back to top »
May 26, 2009 -- 12:05am EDT Women's Heart Health at Stanford
One specific area where Dr. Tremmel recently has made changes, and this was the focus of our interview, was in the vascular access site she uses in catheter-based procedures. She notes that women have higher rates of bleeding complications than men when the femoral (groin) access site is used -- and it is used in more than 90% of procedures in the U.S. This increased bleeding risk prompted Dr. Tremmel to examine, learn and utilize the radial (wrist) approach to angioplasty. She now tries to perform 100% of her procedures through the wrist and, as a result, has had virtually no complications. More information about Women's Heart Health at Stanford can be found here. My full interview with Jennifer Tremmel can be found here. « permalink » « send comment » « back to top »
May 6, 2009 -- 4:05pm EDT Plavix PPI Study Released But a study released today at the SCAI annual meeting showed a greater than 50% increase in major adverse cardiac events in stent patients who were taking both clopidogrel and a PPI. The message was that PPIs have probably been over-prescribed for this particular patient population. The recommendation to patients was to consult their cardiologists, and not unilaterally change their drug regimen (and specifically not to stop taking Plavix -- early cessation of clopidogrel carries an increased risk of stent thrombosis which can lead to heart attack or death). The recommendation to physicians was to look more carefully at why each individual patient might or might not benefit from a PPI, but probably not to give it prophylactically -- and also to return to an earlier class of drugs, called histaminergic (H2) blockers (Zantac, Tagamet) or even common antacids. Of course, a reader of an earlier posting on this blog, D.B. who is a pharmacist in California, already figured this out for himself. Oddly enough, the incidence of gastrointestinal bleeding that required hospitalization was very low across the board, but numerically lower in patients who were not taking PPIs. « permalink » « send comment » « back to top »
May 4, 2009 -- 12:45pm EDT Effectiveness in Stenting
Huennekens' piece was titled, "Obama effectiveness proposal: a tool for finding faster, less expensive medical solutions? " and he details why he agrees with and supports President Obama's decision to study "comparative effective research" -- primarily because there are a number of ways that new technologies, many of them (of course) manufactured by his company, will be useful for interventional cardiology.
Another is Fractional Flow Reserve (FFR) which can measure whether or not a blockage seen to be significant on an angiogram is in fact obstructing blood flow, and how much. The recently published FAME study, detailed in our piece, "Better Outcomes for Stents When Fractional Flow Reserve (FFR) is Used", showed 28% reduction in major cardiac events when FFR was used to determine which blockages to stent and which to leave alone. Also one-third less stents were used: more effective therapy and more cost-effective too. We continue to cover other areas where the effectiveness of catheter-based therapy can be improved. Our Transradial Access Center details the ways in which bleeding complications can be reduced, just by changing the access site for diagnostic and interventional procedures. And we're closely following the use of other imaging modalities, like Cardiac CT angiography (CCTA) which shows promise in eliminating a significant number of invasive diagnostic caths by accurately ruling out coronary disease -- and Optical Coherence Tomography (OCT) which may help in determining stent strut coverage and whether it is safe for the patient to stop taking antiplatelet drugs, such as Plavix. Innovation in medicine may not only be cost-effective, it may be profitable as well. In an excerpt from The Wall Street Transcript's annual Medical Device issue, Matt Dolan of ROTH Capital Partners predicts that, counter to some companies, Volcano is looking at a continued growth rate of 20%. Very effective, indeed. (By the way, the photo posted with Scott Huennekens' op-ed on the Washington Times web site is NOT Huennekens, but Montana Senator Max Baucus -- go figure.... Huennekens is pictured correctly at the top of this article.) « permalink » « send comment » « back to top »
May 1, 2009 -- 4:30pm EDT Comparative Effectiveness Research and
The Patient But in the short term, here are a few quick looks. In March we posted an article about the SYNTAX study which compared bypass surgery to stenting in multivessel disease. The results were not a "yes or no", but more nuanced. Surgery was still the preferred treatment for patients with severe multivessel disease. But for patients with less severe situations, stenting was just as effective ("comparative effectiveness") -- in fact, the authors cited patient preference as an important decision factor. We quoted Dr. Elizabeth Nabel, Director of the National Heart, Lung, and Blood Institute (NHLBI):
This concept of a partnership between the patient and physician is echoed in an op-ed piece in today's Baltimore Sun by Ruth R. Faden and Jonathan D. Moreno. Titled "Power for Patients: Comparative effectiveness research will help people make better health choices", the article emphasizes the importance of patients' control over their treatment, but in tandem with their physicians, and based on the most current information:
We at Angioplasty.Org concur. Each month, 30,000 readers visit our Cardiology Patients' Forum, looking for the latest information to help them make complex decisions. We always encourage those readers who post questions to discuss the information they find with their physicians. One thing we have found, and this is backed up by research:
That is why, at Angioplasty.Org, all of our articles are available to all readers, whether patients or healthcare professionals -- to help foster the partnership that is so critical for "effective" treatment. Comparatively speaking, that is. |

 Back
in January, I
Back
in January, I  Aside
from stents themselves, there's a whole toolbox of devices and
techniques that are candidates for "comparative effectiveness" in
that they may be able to increase the success of interventional
procedures -- or even target patients who need these procedures
more accurately. As Volcano Corp.'s CEO Scott Huennekens wrote
in a
Aside
from stents themselves, there's a whole toolbox of devices and
techniques that are candidates for "comparative effectiveness" in
that they may be able to increase the success of interventional
procedures -- or even target patients who need these procedures
more accurately. As Volcano Corp.'s CEO Scott Huennekens wrote
in a 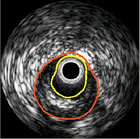 Among
them is intravascular ultrasound (IVUS) which shows more accurate
information about stent placement and expansion than can be seen
on an angiogram. Last July Angioplasty.Org posted an article titled, "
Among
them is intravascular ultrasound (IVUS) which shows more accurate
information about stent placement and expansion than can be seen
on an angiogram. Last July Angioplasty.Org posted an article titled, " More
than a billion dollars has been allocated to "Comparative
Effectiveness Research" in the U.S. Federal government's
stimulus package, yet the term continues to be confused with "cost-effectiveness".
They are not the same, and in an attempt to clarify the difference,
Angioplasty.Org will be posting a number of articles and interviews
in the near future about these issues: specifically how they
impact the field of interventional cardiology.
More
than a billion dollars has been allocated to "Comparative
Effectiveness Research" in the U.S. Federal government's
stimulus package, yet the term continues to be confused with "cost-effectiveness".
They are not the same, and in an attempt to clarify the difference,
Angioplasty.Org will be posting a number of articles and interviews
in the near future about these issues: specifically how they
impact the field of interventional cardiology.