![]()
<< To Homepage >>
<<Archives>>
March 2010 Archives:
March 29, 2010 -- 7:30pm EDT Does Less Angioplasty in Women Having a
Heart Attack Lead to Worse Outcomes? One possible reason was given by Dr. Rita Redberg, a cardiologist at the University of California, San Francisco, as reported by theheart.org:
Dr. Schiele agreed and speculated whether the rates of angiography and angioplasty in women could be safely increased with better stents for smaller arteries, greater use of radial (wrist) access and better antithrombotic regimens. Almost to answer the question, the current issue of Cardiac Interventions Today features two articles on the transradial approach. "The role of radial artery access in the evolution of percutaneous angioplasty and in minimizing complications" specifically discusses how the use of the radial approach in patients with acute coronary syndrome (ACS) and heart attack virtually eliminates procedural bleeding complications, complications which have been associated with increased mortality.
As a result, Dr. Tremmel flew to New York, took a transradial course with Dr. John Coppola, went back to Stanford -- and now does almost all of her cases via the wrist with hardly any bleeding complications. And with increased outcomes for her female patients. Any cardiologist or fellow interested in the transradial approach should definitely check out Dr. Tremmel's recent article. « permalink » « send comment » « back to top »
March 11, 2010 -- 10:10pm EST Three Months of Plavix After Stent: When
Less May Be More A little background: from 2003-2006 patients were given six months of Dual AntiPlatelet Therapy (DAPT, usually Plavix plus aspirin) after getting a drug-eluting stent to prevent blood clots (stent thrombosis) from forming inside the stent. It was assumed that after six months, the stent struts would be covered and thrombosis, would not be an issue. Then came "the firestorm" of the 2006 European Society of Cardiology meeting where papers were presented showing a risk of very late stent thrombosis six months, a year, two years after stenting. The interventional community was thrown into shock and this issue was debated in every meeting, culminating in a two-day FDA panel on stent safety. Following this meeting, new guidelines recommended 12 months minimum of DAPT and more, if patients were not experiencing any adverse effects (bleeding being the main one). But, as Dr. Eric Topol told me in his interview, this recommendation wasn't based on scientific data, because there wasn't any -- it was an intuitive decision that more DAPT would reduce this new found albeit infrequent problem of late stent thrombosis. So the idea of designing a 3,000-plus patient trial testing whether three months of DAPT is sufficient goes against this intuitive concept. Well, things are different. in 2006 there were only two DES: Taxus and Cypher. And Dr. Feres gives his patients 12 months of DAPT when he uses those, except that he rarely uses those. Mostly he is using the second-generation Endeavor stent from Medtronic which numerous imaging studies have shown to "heal" more quickly. OCT imaging has shown almost 100% strut coverage at 3-6 months, even better than bare metal stents. And Dr. Feres has been giving patients only three months of Plavix and aspirin with no problems so far. So the OPTIMIZE Trial, taking place in 30 centers in Brazil will see if there is any difference in three or twelve months. If three months turns out to be "as good", it will actually be "better" and here's why. Plavix costs $4/day. That's $1,100 per patient better. Plus, there are bleeding and other complications associated with Plavix and aspirin. It's estimated about 5%. Hospitalization, transfusions, not to mention poorer patient outcomes. Eliminating those -- that's also better. Finally, patients who get stents also often need other surgeries: dental surgery, knee replacements, biopsies, etc. and many of these procedures are difficult or impossible to do when the patient is on Plavix and aspirin. Reducing the DAPT period to three months reduces this problem as well. For more on the OPTIMIZE Trial, read my interview with Dr. Fausto Feres of Instituto Dante Pazzanese de Cardiologia in São Paulo, Brazil. « permalink » « send comment » « back to top »
March 3, 2010 -- 3:50pm PST Functional Measurement Functioning Well
at Volcano And if the company's results are any indication, both technologies are increasingly finding a place in the interventional cardiologist's armamentarium. Volcano's sales of IVUS catheters were up 29%, but their FFR product was up a whopping 92% over the previous fourth quarter. One reason might be the increasing evidence that FFR or Functional Measurement (FM) is a valid decision-making technology. A major driver for heart docs to look at FFR was last January's FAME study, which showed better outcomes (and fewer stents placed) when FFR was used to guide treatment and ensure that stenting was a benefit for the patient. The strength of IVUS is more in the area of performing the stenting procedure optimally. I wrote about the differences between these technologies a few weeks ago (IVUS vs. FFR -- Boston Style) but these sales figures translate to increased adoption of technologies to make angioplasty, stenting and PCI procedures safer for the patient with better outcomes for the procedure. |
 The
second article, "
The
second article, " "All
stents are not the same," Dr. Fausto Feres told me
in
"All
stents are not the same," Dr. Fausto Feres told me
in 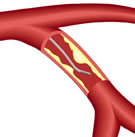 To
stent or not to stent? The question is more than a rhetorical
one when a patient is on the cath lab table and a coronary blockage
is seen on the angiogram. Luckily, there are methods available
to help give a more scientific answer to this question. Equipment
for two of these techniques, Intravascular Ultrasound (IVUS)
and Fractional Flow Reserve (FFR -- a.k.a. "functional measurement")
is manufactured by Volcano Corporation (Nasdaq: VOLC) a San Diego-based
device company that announced its
To
stent or not to stent? The question is more than a rhetorical
one when a patient is on the cath lab table and a coronary blockage
is seen on the angiogram. Luckily, there are methods available
to help give a more scientific answer to this question. Equipment
for two of these techniques, Intravascular Ultrasound (IVUS)
and Fractional Flow Reserve (FFR -- a.k.a. "functional measurement")
is manufactured by Volcano Corporation (Nasdaq: VOLC) a San Diego-based
device company that announced its