
|
|
|
 |
 |
 |
Angiograms: Shadow Images
The images that we see form a construct in our brains of what may
be reality. For half-a-century, the two-dimensional shadow images
of the coronary arteries,
as served up by the "gold standard" of selective coronary angiography,
have informed cardiologists as to what a stenosis is, how severe it is, where
it stops, starts, what it's composed of and, perhaps, how to best treat it. |
|
But newer intravascular imaging modalities have challenged those
black-and-white renderings, and have offered a more accurate image
of what in fact is going on inside the coronary arteries: accuracy
that has resulted in better outcomes for patients and potentially
lower healthcare costs due to less repeat procedures.
The diagrams to the right show an actual
LAD
blockage and an artist's rendition of the same..
Certainly that fluoroscopic shadow image can be measured, comparing
the narrowed area to what looks like the full size of the
artery
before and after the blockage. And
it can be pronounced an 80% or 90% stenosis. This is, however,
a measurement of the image, not necessarily of the arterial blockage
itself, because the angiogram
is, in essence, a two-dimensional "shadow image" of the
artery.
|
|

Coronary narrowing,
as
seen on angiogram (top)
and artist's rendition
of the same |
|
For example, what if this blockage, or
stenosis, were eccentric? What if viewing this artery from a different
angle showed less (or more) narrowing because the blockage
was oval-shaped in the extreme? What if the disease actually spanned
a greater length than the angiogram showed? What if the entire
segment of the artery were diseased and the native arterial
diameter was actually wider than the angiogram showed?
These are all situations
in which the angiogram may or may not show the accurate picture
of what is going on inside the artery. And misjudging the diameter
and length of the blockage may lead, for example, to undersizing
a coronary stent to be placed. More on this later....
|
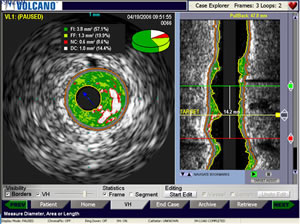
Intravascular
of artery (left) and
reconstruction (right) |
|
IVUS: Imaging
the Artery from the Inside Out
Enter intravascular imaging and guidance, in the
form of intravascular ultrasound, or
IVUS. An ultrasound imaging device is quickly threaded over a wire
and through the catheter that injected dye for the angiogram. A special
"ultrasound camera" is able to see through the plaque and
determine where
the
actual native wall of the artery would be (if the plaque were not there).
This same "camera" also images the plaque itself --
and with some systems, such as VH-IVUS, is able to characterize
the plaque (hard,
soft, calcified,
lipid-rich, etc.). The IVUS imaging device is then "pulled back"
through the entire arterial segment, generating a rapid series
of cross-sectional images which are quickly processed into a longitudinal
reconstruction of the artery.
|
|
As can be seen in the above image, the
IVUS reconstruction is not a shadow image, but an extremely precise
and measurable roadmap to the artery. The software quickly measures
the
diameter and length of the blockage and tells the cardiologist exactly
the diameter and length of the stent he will need to optimally open
this blockage.
Which brings us to the "IVUS State of Mind"....
|
|
IVUS First Identified a Major Problem with Stents
At the beginning
of the stent era, problems began to arise with excessive restenosis
(re-blocking of the artery) and stent thrombosis (blood clotting
inside or around the area of the stent). IVUS was, at that time,
a very new imaging modality. And one of its proponens was Milan-based
Dr. Antonio Colombo. He used IVUS imaging before and after stenting
and looked at patients where the results of the stent had been poor.
And what Colombo found has changed the way stents have been deployed
ever since.
|
|

Antonio Colombo,
MD |
|
When stents first came into widespread
use, cardiologists understandably were overly cautious with this
new technology.
They
were afraid to
expand the stent too far
for fear of over-expanding and tearing the artery.
But Colombo's
IVUS images showed that many, if not most, stents were being underexpanded,
underdeployed -- that they weren't being fitted snugly against
the arterial wall. The result of this underexpansion was that the
spaces
between the stent and artery wall became areas susceptible to platelets
collecting and forming clots, or tissue growing and causing restenosis.
Like an ill-fitting door or window, the space around a too-small
stent was causing the exact problem it was trying to eliminate.
So cardiologists began using high-pressure balloons to expand
the stents fully. And the only true way to measure the exact diameters
and lengths was to use a technology like IVUS. If the cardiologist
knows the precise size of the artery and the blockage, he or she
can size the stent correctly and expand it fully...and safely...without
worrying that the stent is going to overdilate the artery. And
to make sure that the stent is long enough to cover all the disease
(implanting a stent edge in a diseased area is a sure way to cause
reblockage later on).
Just as angiography first gave doctors a way to think visually
about the coronary arteries, intravascular imaging modalities like
IVUS
are now giving cardiologists a new, more complex and more accurate
way to "see" and treat coronary artery disease: an IVUS state of
mind.
In our interview
with Antonio Colombo,
we asked him if he uses IVUS on every single case. His answer
was, as follows:
"Almost all. It depends. In a public hospital sometimes
I am pushed by the schedule, by the patient load, so sometimes
I have
to make
some practical decision. If the lesion is very simple, I
cut short. But still, having used IVUS most of the time,
I have
acquired
what you might call an IVUS background, an IVUS mentality....
So I always think of the vessel as a little bit bigger than
the way it looks. But Ive been working in this field for
more than 25 years, so sometimes I assume that I know...."
|

Shigeru Saito,
MD |
|
Taking an IVUS image adds only
minutes to the procedure and studies show a correspondance between
IVUS use and lower rates of restenosis and thrombosis. Take, for
example, the experience of Japan, where IVUS is completely reimbursed
by insurance and
so is used
in virtually
every PCI. When randomized clinical trials of new
stents are published, the Japanese cohorts always show lower rates
of complications.
So Angioplasty.Org asked Dr. Shigeru Saito, principal
investigator for many of these clinical trials and studies, why
this is the case? Why are the Japanese results always better?
His answer? IVUS!
|
Reported by Burt Cohen, September 24, 2011
|
|
|
|