|
|
 |
Angioplasty.Org
recently talked with Dr. Ron Waksman, Associate Director,
Division of Cardiology at the
Washington
Hospital Center (WHC) and Director of Experimental
Angioplasty & Emerging Technologies for the Cardiovascular
Research Institute(CRI) at WHC in Washington, DC. With over
25 years of experience in leading-edge medical technologies,
Dr. Waksman is a world-renowned interventional cardiologist
and is a highly sought after principal investigator for pre-clinical
and clinical studies conducted in the United States and abroad.
His current research interests include intravascular ultrasound,
bioabsorbable and biodegradable stents, lipid sciences, and
gene cell therapy.
Dr. Waksman has authored/co-authored 310 published manuscripts,
over 230 abstracts, more
than 20 book chapters and has been editor/co-editor of six
books in the field of cardiology. He serves as the Editor-in-Chief
of the journal Cardiovascular Revascularization Medicine (Including Molecular Interventions) and is on the editorial
boards of numerous scientific journals including Circulation,
Journal of American College of Cardiology, and American
Journal of Cardiology. |
|
 Ron
Waksman,
MD, FACC
Ron
Waksman,
MD, FACC |
 |
|
Co-Director of the Interventional
Cardiology Fellowship Program at WHC, Dr. Waksman also runs
the annual Cardiovascular
Revascularization Therapies (CRT) meeting, an event that
presents more than a dozen concurrent scientific meetings
to medical and industry professionals in the field of cardiology.
CRT2009 will
be held March 4-6, 2009 in Washington, DC. |
| Q:
Your group authored a study, which was published online
in the June 11 issue of the European Heart Journal. The
paper is titled, “The potential clinical utility
of intravascular ultrasound guidance in patients undergoing
percutaneous coronary intervention with drug-eluting
stents" (read
abstract). To summarize, what were the major conclusions? |
Dr. Waksman: We wanted to
ask the question of whether systematic IVUS guidance of DES
implantation results in better outcomes, meaning less stent
thrombosis and perhaps also less repeat revascularization.
The results of the study supported this hypothesis:
"if you do IVUS for most of your patients, you're
probably going to end up with better results, as opposed
to non-IVUS
guided PCI
with DES."
What prompted this whole research initiative
was the fact that when we had been looking at patients
with stent thrombosis initially and, when we tried to look
at predictors for stent thrombosis, what always came up
was the lack of IVUS use. So that actually prompted us
to look at more comprehensive sets of patients, and to
ask this as a direct question, rather than to bring it
up as a predictor for stent thrombosis.
|
|
 |
Q: So this was an observational study?
Dr. Waksman: It was observational. It was a retrospective analysis
obviously, but there was a large cohort of patients initially
entered into the database of the study to analyze and address
this question -- our center uses IVUS in
nearly 70% of our patients. We also recognized that there
could be some limitations, because the potentially more difficult
patients would undergo
more IVUS than the simpler ones, or the simpler ones would not
undergo IVUS at all.
So we did a very careful propensity-score matching
analysis, which trimmed the 2,000 some patients to 800, split more
or less evenly
between the groups. The nice thing about it was that we got a very
nice matching between the two groups: those who had IVUS versus
those who did not have IVUS, in terms of baseline characteristics,
in terms of angiographic characteristics, in terms of indication
for use, in terms of the procedures that were done, everything
was very well matched. And the only difference at the end of the
day was the lack of IVUS in one group versus the use of IVUS-guided
PCI in the other group. I think that's strengthened the results
of the paper which do indicate that, with the broad use of IVUS,
there is a reduction of stent thrombosis and also surprisingly,
or maybe not surprisingly, also reduction in the need for repeat
revascularization.

Washington
Hospital
Center |
|
Q: There have been
previous studies, showing better results with bare metal
stents, but I think this is the first study that looked
at drug-eluting stents?
Dr. Waksman: Correct. This study was directed just for DES. Again, it's
not a prospective study, but it's the largest retrospective observation.
And it's a pretty large number, I mean if you're taking into account the
amount of IVUS that is being used, and it's used so selectively. I think
the difference in our center is that we use nearly 70% IVUS in our interventions.
We can do this kind of analysis because we have enough patients, as opposed
to centers that do only 12 or 15 or 20%, which is not sufficient numbers
to do such a study. |
Q: Based on your observations then, do you recommend greater IVUS
use, generally speaking? And does every case need IVUS, or can
IVUS really be targeted to more specific situations, such as more
complex anatomy, etc.?
Dr. Waksman: I do think that it does help across the board, but
obviously it is more helpful in more complex lesions. So, for example,
there are some situations in which IVUS tells you a lot: for example,
in-stent restenosis. If you want to know whether this is a mechanical
issue versus a tissue issue, IVUS is very helpful.
If you go to selection of length and size, that applies to every
lesion. Even if you think that you know the size, you may be surprised
that you are not exactly accurate just by doing angiography alone.
And also it does help you if you need to make a decision whether
to do plaque modification versus direct stenting, for example.
So there are a lot of helpful
hints that you can get from IVUS. But perhaps the most important
one applying to the drug-eluting stent is to obtain sufficient
cross-sectional area after deployment of the stent.
So, not
only verifying by angio that you got a good result, but to
see that indeed the stent is well-expanded, and also well-apposed
to the vessel wall. But I think the emphasis is on expansion,
because sometimes you can miss on the expansion of the stent
without an IVUS. Again, I think systematic use of IVUS post-stenting,
enabling you to ensure expansion, to get the ideal cross-sectional
area, probably will you get you out of trouble or may in
the future. |
|
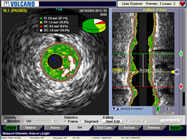
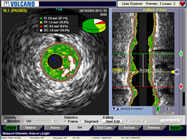
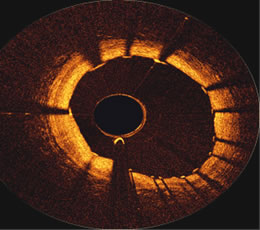
Intravascular
ultrasound image,
courtesy Volcano Corporation |
Q: Your paper concluded that IVUS guidance has the potential to
influence treatment strategies. What I found interesting was that
the IVUS group had less direct stenting, more post-dilatation,
and more cutting balloons and Rotablators were used. Were these
tools and strategies called into play because of what IVUS showed?
Dr. Waksman: Absolutely. Absolutely, because if, for example, you
see that this is not a very calcified lesion and you can go with
direct stenting, you can save a predilation balloon, you can save
any ablative devices. Contrary if you see that you have calcification,
but if you can not even cross with an IVUS catheter, you would
direct yourself more towards rotational atherectomy, and you may
end with better expansion of the stent because of the plaque modification
with rotational atherectomy. So these are two examples where IVUS
can change your decision.
Also, I think in terms of strategizing the length of the stent,
the positioning of the stent, and there's of course branching.
For example, in bifurcation lesions, it would be almost essential
to have IVUS, if not before, definitely post, primarily when you're
dealing with two stents. You want to make sure that they're very
well-apposed. It also can determine whether you need to do post-dilatation
or you were happy with the cross sectional area that was obtained
at a high pressure. It's also taught us to go with high pressure
with drug-eluting stents more than we have used before bare metal
stents. So there are many hints that even an experienced operator
can be getting from the use of IVUS to optimize the outcome.
Q: The drug-eluting stents used in
your study were mostly either Cypher or Taxus. Now second-generation
stents, like the Endeavor and, when it’s
approved, the XIENCE stent, are becoming available. Do you see
less of a need for IVUS with these newer
stents?
Dr. Waksman: I don't think so. It's true that this study was done
with only Cypher and Taxus, and the other stents have maybe better
profile and they also have different compliance curves. We would
need to learn exactly how to handle them in the lab, and in terms
of the assessment of the lesion before, I think you still need
to have it. We don't have much experience with IVUS on the new
stents, but you'd like to make sure that you get good expansion
and apposition with also a second generation. So I think the role
of IVUS will be there to stay: it's still very helpful to give
you more confidence in what you're doing, what you're obtaining
at the end of the procedure.
Q: Regarding the second-generation
stents, we recently interviewed Dr. Shigeru Saito, the principal
investigator for the Japanese
arms of both Endeavor and XIENCE stent trials, and his results
were better than the other arms of the studies, something he attributed
to the fact that in Japan, IVUS is fully reimbursed and used on
almost every case.
Dr. Waksman: Yes. I think there is one more study that's coming
from Asia in which they looked at the left main, whether it was
assisted with IVUS or not assisted with IVUS and I think they reported
a sub-study that demonstrated that use of IVUS for the left main
was associated with improved results when compared with those who
underwent stenting without the use of IVUS.
Q: I was surprised to see that there was a three-fold reduction
in stent thrombosis at both 30 days and 12 months with the IVUS
group. The non-IVUS patients had three times the thrombosis. Is
this correct?
Dr. Waksman: Yes, that's true. I think that again, it was unexpected
to see because the rate of stent thrombosis is generally not so
huge, yet it was a difference which was very impressive. And I
think it's for real.
Q: There was no significant difference
in late stent thrombosis, so we’re talking about the type
of thrombosis that occurs in the earlier stages?
Dr. Waksman: Yes, and this applies to the mechanism of stent thrombosis.
I think we better understand that the 30 day stent thrombosis,
which is more mechanical and related to the apposition of the stent,
as opposed to the very late that is maybe more related to healing,
inflammation, and perhaps also to issues related to responsiveness
to Plavix. So I think since the majority of the stent thrombosis
in the first year occurs within the first 30 days. This is the
most important part that we can influence and reduce further. But
I would still question whether the very late stent thrombosis would
be impacted by the use of IVUS. Maybe, but we couldn't prove it
in this study.
Q: What about tissue characterization?
There’s been a lot
of talk recently, unfortunately brought about by journalist Tim
Russert’s untimely death, about vulnerable plaque and plaque
rupture. Can IVUS help in this area?
Dr. Waksman: I think there is still a controversy about the ability
to detect a vulnerable plaque with the current system, because
with IVUS you can see multiple plaques that would be under the
category of vulnerable, but we don't know if any of those are really
going to be turned to a ruptured plaque, and that has not been
proven yet. And yet, should you have this information, what type
of therapy can you do? Let's assume you see 15 or 20 of those,
which potentially you can see with IVUS tissue characterization,
does that mean you're going to treat 20 spots with stenting?
It is important that it has raised this interest in continuation
of exploring how to diagnose or to treat or to prevent vulnerable
plaques to erupt. I'm not sure how much IVUS can help us alone,
but I would say that there are an array of other devices that would
be adjunct to IVUS that would tell us a little bit more about say,
for example, the lipid composition within the plaque, the amount
of inflammation, the necrotic core, the TCFA, the thin cap fibroatheroma,
so all those may be features that may put the patients more at
high risk vs. low risk. What we're missing now is the completion
of the natural history study; we're missing the therapy right now
that we can advocate to make a change in this. So it's the next
step to see a little bit more. But I'm not sure at this stage we
can state anything that could have prevented tragedies the like
one that we had with Mr. Russert.
Q:
What about other intravascular imaging technologies that
can see lipid cores and such? For
example, Optical Coherence Tomography (OCT) has been talked
about.
Dr. Waksman: In terms of the imaging, there is a new
infrared system that has just recently gotten 510k approval
from the FDA and it's going to be commercially available soon.
And that device can allow you to detect the amount of lipids
within the plaque, so that's an interesting approach. Again,
I don't know what to do with it, but it's there. OCT is being
now moving to a more user-friendly system, and it has capabilities
again to detect areas of necrotic core, and there's a lot of
progress in that. There is also IVMRI which also can help detect
lipid content within the plaque, and it has completed the clinical
trial. And there are some other modalities that are being developed
right now to enable us to get a little bit more information
on plaque composition in potentially more high-risk patients.
So I think its a dynamic field and we should look forward
carefully on other modalities, but I would caution that those
have to be integrated all in one catheter, because, as an interventionalist,
you don't have the time to pull two or three catheters to get
all the modalities systematically in every patient -- that's
going to be almost impossible. |
|
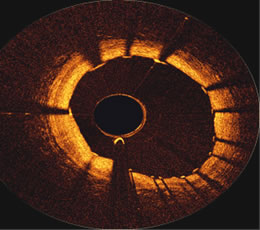
OCT image
just proximal to a stent in an RCA,
courtesy of the First
in Man Volcano OCT
performed
at ThoraxCenter in Rotterdam
by Prof. Patrick Serruys
and Dr. Evelyn Regar |
Q: In the U.S. and other places, IVUS usage is only in the teens.
Would your recommendation be that interventionalists start thinking
about using IVUS more?
Dr. Waksman: I would think that 13% is not sufficient, so there
is room to be more liberal with the use of IVUS. The excuse that
it's cumbersome is fading slowly because we have now integrated
systems, so I think that at this point this is becoming a more
essential tool and there are really not many complications associated
with it. As to it being time-consuming, it's also becoming relatively
simple to use. So I would encourage cardiologists to use it more,
just based on those results because, now that we've been published,
I think that this is an opportunity for even good operators to
end with better outcomes. And if that's the case, then it's definitely
important also for those who feel less comfortable in the cath
lab with complex angioplasty. Here we have a tool that can optimize
your result and you should not spare it on the patient.
I think that this is kind of a wake-up call to people to look
again. I think that's the message from the paper: maybe there's
something there that we can do better and maybe we should give
it a try. From my own experience, and this is more anecdotal, those
who use IVUS a lot don't usually want to give it up, they continue
to do IVUS. And it's just a question of passing the barrier to
start to do it, or a learning curve, or confidence in the device.
But once you start to do IVUS it's kind of something that you like,
it's not an addiction, but I don't know many of those individuals
that used to do a lot of IVUS and stopped doing it.
Q: Thank you, Dr. Waksman. We look forward to
your CRT2009
meeting. Will you be running training sessions for
IVUS?
Dr. Waksman:
You're welcome. And yes, there is an IVUS workshop at CRT. Its also in other
courses, and also from time to time we have a group of technicians and physicians
that
come to the cath lab for training.
This interview was conducted in June 2008
by Burt Cohen of Angioplasty.Org.
|