|
Now, an ancillary study of the FAME data, has been published in the June 22 issue of the Journal of the American College of Cardiology and, as the authors conclude:
Angiography, long considered the "gold standard" in diagnosing coronary artery disease, is now being labeled as inappropriate and inaccurate by those who are utilizing a new technique for determining ischemia. (The authors also note that noninvasive stress testing is similarly inaccurate in determining ischemia in multivessel disease.)
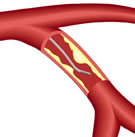
The FAME study refuted this methodology for patients with multivessel coronary disease (narrowings in more than one artery). Using a catheter to measure the blood pressure on both sides of the blockage, called the fractional flow reserve (FFR), cardiologists were able to determine more accurately whether the plaque build-up was actually causing significant ischemia (loss of blood flow). When guided by FFR, less stents were placed and outcomes for the patients were better by 28%, when compared to stent placement guided only by the angiogram. What the authors of this week's JACC paper have shown is that the advantage of FFR-guided stent placement exists not only in what might be called "intermediate lesions" of 50-70% (as measured by angiography) but also in more severe blockages. Two-thirds of the coronary narrowings in the 50-70% range were measured by FFR as being functionally insignificant. In other words, only one out of three blockages in this range was causing ischemia; placing a stent in two-thirds of these lesions was not only unnecessary, but could result in more adverse events. However, even in the more severe range of 71-90% blockages, one out of five stenoses were measured by FFR as being functionally insignificant -- no stent needed. It was only in the range of 91% or greater narrowing that virtually all of the lesions were significant and the patient would benefit from stenting. The implications of these studies are wide-ranging. The authors show that many patients diagnosed with triple-vessel disease may in fact only have one or two vessels causing a problem. They also note that if many of the angioplasty vs. .surgery studies had used FFR instead of angiography to determine whether or not to use a stent, the improved results may have favored angioplasty more. Likewise, the COURAGE trial may also have shown a greater benefit for angioplasty and stenting.
Until now, that is. Today, specialized FFR catheters are manufactured by two companies: Volcano Corporation and St. Jude Medical (which funded this week's JACC study, as well as the original FAME trial). But despite the clear advantages shown in these studies, FFR is still only utilized in 10-15% of all percutaneous coronary interventions (PCI). Both companies feel that this is changing and that, with the advances in design and the integration of FFR technology into the cath lab, this new diagnostic tool will be adopted by cardiologists in increasing numbers, resulting in better outcomes for patients and potentially lower costs (less stents) for the healthcare system. Reported by Burt Cohen, June 23, 2010 |