![]()
<< To Homepage >>
<<Archives>>
April 2009 Archives: April 21, 2009 -- 5:15am EDT CT Scans for Strokes It's an important topic, and one which Dr. Nick Hopkins, head of the Toshiba Stroke Center, discusses in more detail during our interview, posted in Angioplasty.Org's Imaging and Diagnosis Section. Stroke has been called a "heart attack in the brain". If only it were that simple. A heart attack is caused by a sudden stoppage of blood to the heart -- the treatment: open up the blockage. But strokes can have two different causes -- and the treatments for these two different types of stroke are totally opposite. An ischemic stroke, the "heart attack in the brain" type, is treated with clot-busting drugs, and/or a clot-retrieval device, threaded to the brain via a catheter, not unlike angioplasty. But the second type of stroke is caused by an aneurysm or other type of bleeding complication. Giving a clot-buster in this situation would be disastrous. Luckily, a CT scan of the brain immediately tells the physician which type of stroke the patient is having. And luckily again, CT scans can be done very quickly in an Emergency Department set up for this type of diagnostic procedure. Furthermore, as Dr. Hopkins points out, there's yet another advantage to the CT scan -- it also shows the viability of the brain tissue. If significant parts of the patient's brain tissue have died, attempting to reperfuse (increase circulation) in those parts may cause even worse complications, such as hemorrhage. The controversy detailed in Burton's article is over official guidelines for the use of CT, with implications for reimbursement. I won't get into the details, because you should read his piece, but this is just one more issue where advances in imaging, being able to see, have profound implications for being able to treat. « permalink » « send comment » « back to top »
April 18, 2009 -- 10:45pm EDT Plavix and PPIs: Update So earlier today reader D.B., a pharmacist in California, sent in this:
In fact, there are two recent updates. One is a study in the current issue of Thrombosis and Haemostasis, an official publication from the European Society of Cardiology. The article, "Impact of proton pump inhibitors on the antiplatelet effects of clopidogrel", shows a definite effect in the inhibition of clopidogrel's antiplatelet function when using omeprazole (a.k.a. Prilosec) but, interestingly enough, the other PPIs tested showed no such effect. However, it was a study that measured platelet reactivity and not clinical results, so the other PPIs are still not out of the woods. In fact an editorial in the same issue recommends against the use of PPIs with Plavix (clopidogrel) which goes against the recommendations of the American societies. The second update (or future update) may clear some of this up in a few weeks. New results from the Medco study are scheduled to be presented at the annual SCAI meeting in Las Vegas May 6-9, so we'll be reporting on that when it breaks. It will be interesting to see if guidelines and recommendations will change as a result. As for H2 blockers (like Pepcid) they were by and large replaced when PPIs hit the market. There is question how effective they are in this situation, and they also had some side-effects, but were never shown to inhibit antiplatelet drugs like Plavix. « permalink » « send comment » « back to top »
April 6, 2009 -- 10:00pm EDT Cardiology Sites Taking Notice of the Radial
Approach to Angioplasty and Stenting (PCI) This is interesting on several levels: one, this poll has been posted and open for voting on theheart.org considerably longer than previous polls; two, as of this morning (see graphic above) over 500 votes have been tallied from healthcare professionals who read theheart.org (this is a lot of votes for a typical poll on their site!); and three, the vote is 50/50! -- and has been so over the past couple of months, sometimes going up to 52/48 in favor of radial. This last point, the vote results, is even more interesting because the most recent data from the NCDR database shows that less than 3% of angioplasties done in the U.S. are done via the radial artery in the wrist; the mainstay of catheter-based procedures in this country remains the femoral artery in the leg/groin. (Not so around the world, where 50% or greater is the norm. In fact those cardiologists who are proficient with the radial technique tend to use it in 70-80% of their cases.) So if less than 3% of PCIs are done via the wrist, why is the vote 50/50? Is it because many cardiologists from outside the U.S. have been voting? Or is it because many cardiologists feel that radial should be the preferred access site -- but they just don't practice it themselves? Or, more likely, aren't trained in it? For two years now, Angioplasty.Org has been offering a special section on this technique, our Transradial Access Center, offering information to both physicians and patients about the advantages of the radial approach: less complications, greater patient comfort, cost-effectiveness, etc. And we've also been listing training opportunities, U.S. hospital centers where radial is practiced, interviews with key cardiologists who use it. And we've seen increasing interest in the radial approach as a result. In fact, today the weekly poll on another "professionals only" cardiology site, CRTonline.org, asks the question:
Only 64 votes have been cast at present, and almost half are saying "less than 20%", so it will be "interesting" to see how this goes as the week progresses. So...to you radialists out there, go vote!! Late Update: Alas! theheart.org has taken down its poll -- glad I got a screenshot of the final tally. Later Update: The poll at theheart.org -- is back online!
|

 A
couple of months ago
A
couple of months ago 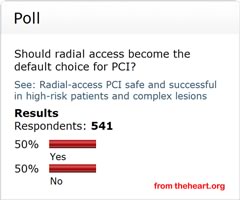 Two
months ago,
Two
months ago,