|
|
|
 |
Dr. Giulio
Guagliumi, an internationally recognized leader in the use
of Optical Coherence Tomography (OCT) in the coronary arteries,
practices in the Cardiovascular
Department
of Ospedali Riuniti di Bergamo in Bergamo, Italy. He
has spoken at numerous conferences worldwide and recently
brought together experts for a course in Bergamo, titled "OCT,
IVUS, FFR: When, Where, How" -- in which the clinical
applications of these technologies were explored and demonstrated.
Dr. Guagliumi has been published in numerous peer-reviewed
journals and is principal investigator in several clinical
trials assessing the performance of stents inside the coronary
artery, using OCT imaging. One recent study, the
ODESSA Trial (Optical coherence tomography
for DES SAfety) was presented at TCT 2008 and was one of
the first looks at drug-eluting stent coverage and healing
inside the artery. OCT imaging, although a very new modality
for interventional cardiologists, is now being utilized by
the medical profession and industry during the early stages
of stent design to assess safety issues of strut coverage.
|
|
 Giulio
Guagliumi, MD
Giulio
Guagliumi, MD |
Q: Much has been written about intravascular ultrasound IVUS and
its usefulness. But optical coherence tomography (OCT) is the new
kid on the block. Where is this technology right now, with regard
to both research and clinical application?
Dr. Guagliumi: When you are working in a new field, opening a new window, you
have a lot of expectation and you need time to realize the level you can reach
in clinical intent. These are spectral technologies. IVUS has been with us for
20 years -- OCT is more recent -- but in either case we are talking about something
that is quickly changing.
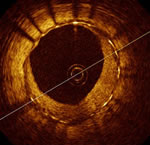
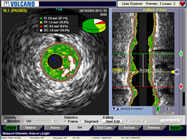
OCT image
from ODESSA
Trial,
showing covered and
uncovered struts of a
drug-eluting stent |
|
We started to use OCT in
the coronary field a couple of years ago. The first group started
to use it to detect vulnerable plaque. Then, and I think this
is one of the merits of my group, we quickly switched to something
that was dramatically more important in clinical use: "Can we
derive information on the coverage of the stent struts and the
healing process?" So we started working with the problem of late
and very late stent thrombosis.
But during the last couple of years this was done with early
OCT technology that was quite difficult to use, because you had
to be quite expert: you had to occlude the vessel and flush away
the blood, just to allow the fibers to have a perfect clean vision
of the vessel. Because, of course, it's a light technology, so
the blood is going to create the problem. So that was done systematically
with very dedicated work for a couple of years. And you needed
a very skilled team, just to have the best images without artifacts
and contamination. |
Today, two years later, we are discussing
the possibility of scanning an entire coronary artery in 3 seconds
and obtaining high quality
images without needing any occlusion. That’s what we showed
at our course. So it's not just one technology. It's something
that is changing extremely quickly. And the level of the clinical
information that we can get is extremely dynamic. We have a lot
of expectation. It is the beginning of the story.
Just comparing OCT with IVUS today, with the current technology
we have at least a 10-30 times higher resolution. We can analyze
one stent not in a few sections, but in hundreds of sections. The
problem is: can we deal with all these data very quickly and very
appropriately without anything in excess? And that is what's going
on -- but a very dynamic situation with a lot of potential improvement
just around the corner. We need time.
Q: Can some of these technologies be used clinically right now?
Certainly IVUS is being used much more than it was. OCT, as you're
saying, is more of a research tool right now.
Dr. Guagliumi: This new technology, where you are able to scan
one coronary artery in 3 seconds, means that you can do this without
a super-expert team. And that could be extremely important. Even
today we are just normally performing many of these evaluations
in stented patients to determine healing. There are papers coming,
probably in one or two months, showing that the correlation with
histology for coverage is very very high -- quite impressive. So
it's going to change the level of understanding in a practical
way of the stent-vascular response.
I can say that when we are discussing late
and very late stent thrombosis, people have in mind that it's
just one single phenomenon.
But it is something that is very complex. Sometimes when you are
using this technology to cut the stents in slices of cross-sections,
in vivo, you may see four different types of responses in only
4mm. So you might have a beautiful stent for 95% and then you can
run into trouble in 2 or 3mm. And that is going to be extremely
helpful to guide us. Number one, to throw out the most toxic technology
and two, all types of investigation in the next generation of stents
is going to include this technology as an early evaluation before
going into thousands of patients with the final release – so
in just a small group of patients there is good information about
the healing process.
What about the clinical practice every day? We have already shown
that OCT is a very sensitive technology for thrombus detection,
for malapposition -- much more accurate. We still have to prove
that all of this information is going to impact the outcome.
Q: With the Horizons-AMI OCT subset
there were some comments, for example, by Dr. Renu Virmani
that you
couldn’t really
tell what types of cells were covering the struts: they might be
fibrin and not endothelium.
Dr. Guagliumi: Of course this is true and it is something we need
to target. As I said before, this is the first step. Light is the
most flexible radiation available. You can use not only the intensity,
you also can use polarization, and you can use spectroscopy to
determine the chemical aspect -- that is the next target. We have
already started with tissue characterization. Until now we used
just one single parameter: the intensity of the signal. And now
we are opening a new phase. But what is important is the first
step: can we scan the entire coronary artery in a short period
of time without asking the people who are doing it to be extremely
expert? Now we can say yes, because now it's a simple procedure.
The next step is the separation between fibrin and neointima --
and then we are going to something even more precise, probably
with spectroscopy.
Q: You've said that
the data coming from these studies may impact the design
of new stents and other new technologies?
Dr. Guagliumi: This concept has been accepted by the European Society of Cardiology.
A little over a year ago, we had kind of a consensus meeting, which has been
published in the European Heart Journal, EuroIntervention.
On the team was Eugene Braunwald, Patrick Serruys, Mitchell Krucoff and many
others, including a web transmission from the U.S. We discussed what is important
for the DES application. And one of the written conclusions for the future was
that we wanted to have more than only QCA data -- although QCA data are very
reliable for restenosis, they are not telling you anything about the healing
process. So the paper recommends that for the future generations of DES, we should
have systematically collected IVUS data and OCT data and endothelial functional
data. That is a sort of an official statement, and the FDA is going to follow
the same pattern. |
|

Dr. Guagliumi
in cath lab |
Q: This would be for approvals in the future?
Dr. Guagliumi: And for checking the level of risk before putting
devices into thousands and thousands of patients.
Q: One interesting outcome from a trial that you did, the ODESSA
Trial, looked at the four different drug-eluting stent types and
came up with some pretty interesting data about the differences
among them.
Dr. Guagliumi: First of all, it is confirmed that DES are not just
one single family. Each one has its own profile. Logically the
more you push the envelope in trying to make zero neointimal growth,
the more you risk leaving some struts uncovered, or some struts
malapposed. So OCT technology is going to dramatically increase
the understanding of the response. As I said before, don’t
think about the stents having an all-or-nothing response. It is
a very sophisticated response from any different site of a single
stent. So it's a spectrum and it depends upon the interaction between
plaque and drugs, concentration, but for sure these stents are
going to be extremely different and you can see these differences
by using this technology.
Q: One striking finding was that strut coverage was much greater
on the Endeavor zotarolimus-eluting stent than with the others.
Dr. Guagliumi: The data fit with all the scientific data previously
published. When you have a late lumen loss on the average of 0.6
for the zotarolimus stent, you have more tissue. But the stronger
message is not that you have more tissue -- it's that you have
a very uniform response. So zotarolimus is very homogeneous, and
I can guarantee that, having seen some very recent graphs.
We also just finished another study -- named OCTAMI. It is the
same use of zotarolimus vs. bare metal Driver in acute myocardial
infarction -- so a different setting, just to see if the same type
of uniform behavior and coverage is maintained in maximal critical
situations such as AMI.
For the other stents, as I said, the concept is heterogeneity.
So the more you are aggressive, the less you have this uniform
response. You might have great section with nice coverage, but
you might have a section that is completely devoid from coverage.
And that's in fitting with the value of the late lumen loss around
zero. So the problem is how we can get the nice balance, not too
much and not too thin.
Q: Have you been able to definitely link uncovered struts with
increased stent thrombosis?
Dr. Guagliumi: Two points. Number one, all the patients in all
these studies are clinically followed up. Just to see the relationship
between the images and the clinical outcome. But in this case we
use the pool of all patients, so we are following ODESSA, we are
following Horizon-OCT, we are following OCTAMI, we are following
OCT-DESI, we are following LONG-OCT, we are following many, many
trials. We need enough numbers.
Another critical point is we need a high quality of images and
that is my major preoccupation. If you have this type of heterogenetic
response, it's not easy to get great images for all the sections,
all the stents, all the patients. And if you are going to deal
with the artifacts, with suboptimal images, perhaps you cannot
be so precise. So we are just trying to put on the paper the concept
of the artifacts, how to try to be as clean as possible and to
have the most reliable data.
But, with hundreds of these patients followed
clinically, and we are already at two years, at the end we will
arrive to see if
there is a relationship. I can anticipate something. I wrote an
editorial
for JACC: Interventions for a paper that was published
in May by a Japanese group, working with Stanford. For the first
time they
showed that uncovered struts are related to thrombus formation.
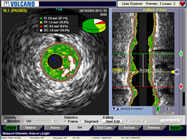
IVUS Study,
courtesy Volcano Corp. |
|
Q: What about the role of
other intravascular technologies, such as IVUS?
Dr. Guagliumi: Just to give you an idea, my last talk at the
ACC during the official OCT meeting was titled, "IVUS is dead." The
title was not my choice! But it gives you the feedback that when
you are pushed, you start to react.
So what we can expect is
a significant improvement in terms of IVUS technology. We already
have a new generation of catheters that can be tracked easily
in the distal part of the coronary arteries with more pushability,
more lubricious. That is one. Then we are going to have a much
quicker pull-back. We are going to have a higher numbers of
frames. |
My idea is that, in any case, light is extremely superior to ultrasound,
to sound waves but, of course, light has limitations such as penetration.
Light has difficulty in going deeply into the tissue. That is the
reason why in all of the studies and all the patients, we used
both technologies in pair. OCT just to get the information from
the internal surface of the vessel which is much more detailed,
but also IVUS to get information about the outside part of the
vessel, remodeling for instance. So this type of combination is
the true projection for the future, because we think that for a
certain period of time, light will remain limited in deeper tissue
penetration.
Q: So a system that allows you to use both OCT and IVUS is helpful.
Dr. Guagliumi: Yes. There are systems already in development that
are trying to combine and be flexible on the table so to have
some very interactive options and to get the best information
possible. As I say, these are very quickly evolving technologies,
so we need to wait and see in which direction they are going.
But in any case, IVUS is going to react giving much better quality,
a larger bandwidth spectrum, higher frequency, so more detailed
information.
Q: And Virtual Histology also?
Dr. Guagliumi: Virtual Histology, yes -- Virtual Histology is one
name, perhaps tissue characterization is another name. The concept
is the same. So with IVUS, the limitation was that we were analyzing
just one single parameter: the intensity of the signal. Then
we went to the analysis of the spectrum and that produced Virtual
Histology.
For us in OCT it was the same. We started with intensity in the
previous generation of OCT; now we are using what is called spectral
domain OCT that is going to have the spectrum of the light that
is millions of times superior to the spectrum of the sound.
Q: Do you foresee OCT technology impacting the use of histology
or pathology in pre-clinical work?
Dr. Guagliumi: We are just transferring this technology to pre-clinical
use. For example, in pre-clinical when you wanted to see a stent’s
response in let’s say two weeks, you needed to take a group
of treated animals and then sacrifice them to inspect the results
using histology. But you will then need to see results at 30 days
or six months, so you have to go back and restart the study with
another series of animals. If we can gain the time dimension, to
have a reliable technology (OCT) that is in line with the histology,
that doesn’t require having to restart and sacrifice animals
each time, you can really see what is going on over time. The need
that we have today, one of the most important, is to have pathologic
animals that are going to mimic what now we know is going to happen
in humans, and use this technology to get the most appropriate
device as soon as possible.
Q: What are the future trials
that will be coming out?
Dr. Guagliumi: We have already finished
OCTAMI -- OCTAMI is just to test if the uniformity of the response
in zotarolimus is the same in acute myocardial infarction as
it was for elective indications in ODESSA. Because, even if
it's off-label, the setting is different and we wanted just
to see if the response was going to be the same.
We have finished
the enrollment and finished the follow-up. It's the identical
platform but one is DES and the other bare metal stents. |
|

Ospedali
Riuniti di Bergamo |
The second study that we are finishing shortly and perhaps will
be submitted to and presented at TCT, is the new ablumenal polymer,
JACTAX vs. TAXUS. LabCoat was recently acquired by Boston Scientific,
and it is not just a polymer wrapping around the entire stent,
but is only ablumenal, on the outside of the stent. Also, in terms
of thickness, the polymer is just one micron thick, compared to
18 microns in TAXUS. So we are finishing the study: the primary
endpoint is OCT and, of course, IVUS. So it is a comparison with
the control arm, but in this case the control arm is the first
generation of the stent. So this is the first prospective randomized
study comparing a new stent generation with the first generation
using OCT as a primary endpoint -- and the name is OCTDESI.
Q: At TCT 2007, OCT was hardly discussed.
But at last year’s
meeting there was a lot of talk about this. Would you say that
the use of OCT is beginning to grow rapidly?
Dr. Guagliumi: Today, every day in Japan they are doing 450 OCT
cases on average. There was nothing until one year ago. Of course
I have a lot of friends in Japan and they are participating in
our meetings as well.
The growth of OCT is explosive. I receive
two or three manuscripts per week for peer review so as I said
before, the preoccupation
is for quality, because otherwise we're going to have conflicting
data. And all the experts are starting to agree on some consensus
documents talking about definition, technology -- it's a technology
that’s growing so quickly, even in terms of the marketing
impact, that we need to guarantee the quality of the data because
it could be a serious problem. But many people are joined; we are
having fluent conversation with our Japanese friends, U.S. friends
and the Europeans; it's probably helping to quickly get an enormous
quantity of data, yet at the same time guarantee a correct analysis.
This interview was conducted in April 2009
by Burt Cohen of Angioplasty.Org.
|