|
|
 |
Dr. Hodgson
is an internationally acclaimed cardiologist who, prior to
founding Santι Cardiology,
was the Chief of Academic Cardiology at St. Joseph Hospital
and Medical Center in Phoenix. Previously
a faculty member at the Medical College
of Virginia and Case Medical School in Cleveland,
he has devoted much of his career to training the
next
generation of physicians. He
has served in many administrative positions and developed
four Cardiology
Departments. Dr. Hodgson is a Past President
of the SCAI and
a founding member of the
SCCT.
He has published over 200 peer reviewed articles, 8 books
or
book
chapters,
holds
two
patents and
developed the TeachIVUS and
TeachFFR online
simulation training tools.
Angioplasty recently sat down with Dr. Hodgson to talk about
intravascular technologies. This interview is posted in two
parts:
- Part One discusses intravascular
ultrasound (IVUS) and how it can increase the accuracy
of stent placement, and the role of IVUS in the era of
DES 2.0;
- Part
Two discusses Fractional
Flow Reserve (FFR) with some thoughts on training and
recommendations
for patients.
|
|
 John
McB. Hodgson, MD
John
McB. Hodgson, MD
Santé Cardiology
Phoenix, Arizona |
Q: Can using intravascular ultrasound (IVUS) for stent placement
really improve patient outcome and reduce late stent thrombosis in
drug-eluting stents?
Dr. Hodgson: There are nine trials
that have compared IVUS-guided bare metal stenting to angiographically-guided
stenting. Eight showed IVUS was superior and one was neutral.
However, because late stent thrombosis is a very low frequency event
(I think Gregg Stone has estimated, it would take upwards
of 20,000 patients per arm to try to estimate a difference)
there is no randomized, controlled, multi-center trial that proves
that IVUS use is better for late
stent thrombosis in drug-eluting stents.

Taxus
drug-eluting stent |
|
But, in terms of stent
restenosis, TLR, acute events, cost-effectiveness -- all
of that stuff's been studied for bare metal stents,
and all of those studies but one, which was neutral, showed
favorable
results for routine IVUS use for stenting.
Now a lot of
people debated whether that would still be true for drug-eluting
stents.
But most of us feel there's no magic about drug-eluting
stents that makes them somehow mechanically superior,
so that you
can basically do a sloppy job, or leave unexpanded stents,
or leave stent malapposition and get away with it because
of the drugs. I don't think anybody believes that now,
and it would just be common sense that you would want
to implant
the device as well as you possibly could in order to
prevent any adverse outcome. |
You have to look at this in a little bit broader terms. It depends
on the tortuosity, the size of the vessel, the type of the stent,
the other risk factors that the patient has: renal failure, heart
failure or diabetes, etc. If you have a complex lesion (and complex
could be small, ostial, bifurcation, calcified) we've learned from
the past 15 years that IVUS use will result in a better acute outcome.
The minimal lumen diameter, the minimal cross-sectional area, however
you want to measure it, it'll be better if you do IVUS guidance
than if you don't. And those differences are more pronounced the
more difficult the lesion sub-set becomes.
I use it 68% of the time, and the more difficult the lesion, the
more complicated the case, the more the patient is at risk for
stent thrombosis, or restenosis, the more likely we are to use
it. So, the 30 year old with a straight shot, mid-right, 4.5 vessel
that's 8 mm long, who's non-diabetic, has no renal failure, no
heart failure, nothing else going on, then you could argue that
it may not make a difference there. But, that's not usually what
we're doing anymore. We're doing much more complicated patients
than that.
Q: Would you comment on the S.T.L.L.R.
study that showed two-thirds of stents are not optimally
placed??
Dr.
Hodgson: I use that study all the time. That's an angiographic
study, not an IVUS study, but we use that to indicate the importance
of the measurements that go into selecting a stent and optimizing
its placement. A lot of it had to do with the stent not covering
the area they had pre-dilated, or not covering all of the lesion.
Those are all things that IVUS could help avoid by properly measuring
the length of the stent, and by ensuring that you've had good coverage
and good expansion afterwards. And in that trial there were more
M.I.s in the ones that had a longitudinal miss, a trend towards
more late thrombosis, and all those nasty things.
Another important trial is one that came out
of Washington Hospital Center, retrospective, Ron Waksman,
looking at over 5,000
stents that they'd put in. One of the important predictors of freedom
from late stent thrombosis was use of IVUS. The use of IVUS and
larger reference vessel size were the two things that correlated
with less stent thrombosis. The other usual predictors came through
as well, so people with smaller vessels and renal failure
were more likely to have stent thrombosis. So it's retrospective,
it's a center that does 78% IVUS use, but the ones
who did well had a higher frequency of IVUS use than the ones who
had stent thromboses.
Q: So IVUS
helps you know you’ve
placed the stent optimally?
Dr. Hodgson:
I've always been amazed that people are happy to throw $3,000
stents in and not really
know for sure whether they've
done a good job or not. Would they buy a set of $3,000 wheels for
their new Mercedes and not care if the guy put them on backwards,
or only used two bolts instead of four? It doesn't make any sense.
You would want it done in the best way possible, and yet, in the
lab they’ll say “Oh, it looks okay, I've got another
case to do. . .”, and the sense that “I don’t
have time” to use a tool that's readily available there,
is just mind-boggling to me. In my lecture, I grill these people.
Some of these studies, there's a 30%, 40% reduction in restenosis
rates. So five minutes of your time is not worth a 40% reduction
in restenosis for your patient? And that's all it takes, five minutes
extra, if you're using IVUS routinely, and have it set up and ready
to go. It's not a big deal.
Q: But we
now have a new second generation of drug-eluting stents – which
I call DES 2.0. Won’t they be better? Do you see the role
of IVUS changing with these newer devices?
Dr. Hodgson:
I don't really. I think that the attention to drug-eluting stents
has been largely focused
on polymers, and different drugs,
and whether you do or don't get in-growth of tissue. But the bottom
line that hasn't changed is that this is a balloon-expandable metal
scaffolding device, and the mechanics of putting that in and getting
it there, has nothing to do with the drug. And I've preached for
years about vessel compliance. You have to understand that the
resistance to expanding a stent has nothing to do with the stent,
and has everything to do with the vessel. So, I don't care what
stent you've got, what balloon it’s on, what name you want
to call it, what drug is there -- if you can't get it in and get
it inflated and expanded in the right spot, it doesn't really matter!
And that hasn't changed. And again, it doesn't make any difference
what the drug is. The drug is going to help you later, but what
you need to do up front, is deliver this thing properly. Put it
in the right lesion, get it to the right size, get it implanted
as best as possible, and then you'll let the drug do its work.
Now, some
of the stents are a little more flexible, so maybe they’ll
be better in terms of getting them there, but there is nothing
magic about these stents in terms of implanting them -- it has
not changed. What we do, in terms of blowing up vessels, has not
changed since the first procedure that Andreas
Gruentzig did. We
have to go in and mechanically push the plaque out the way, and
you
either
do a good job at that, or you don't. If you can get the vessel
wide open, the patients do well. So that's the fundamental issue
here, and Andreas understood it, and many of us have understood
it for years.
All these tools, every one
of them we use, are designed to make the narrow part of the
pipe look like the not-so-narrow part. That's all we do. We
don't make atherosclerosis go away, we don't dissolve plaque
-- all we do is make the narrow spot look like the not-so-narrow
spot. And if you can do a good job at that, then you relieve
ischemia. And that's all angioplasty does: it relieves ischemia.
It doesn't make you live longer, any of that stuff.
I don't care if you've got a balloon, a cutter, a zapper,
a laser, whatever, that's your ultimate outcome. Whether
you want to call the
stent a Xience, or put it on a Vision, it doesn't make any
difference, you still have to make sure that you've got a
good opening, and the only way that you can do that effectively
is with IVUS.
So, I don't care what they develop in the future,
we need a way to ensure that we have mechanically opened
that
vessel in the best way possible, and it depends on the
plaque distribution, the plaque burden, the plaque calcification,
etc., and the only way you can reliably look at that is
with
intravascular ultrasound. |
|
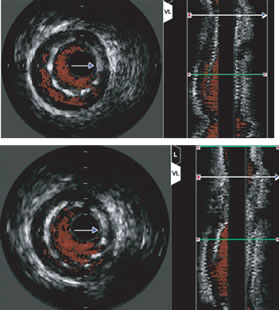
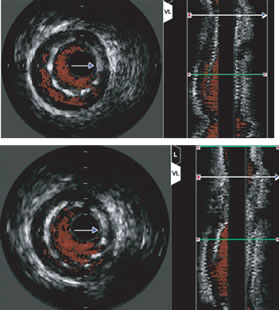
IVUS at
top shows under-expanded stent; at bottom the stent has been
post-dilated with a balloon for a better fit. Both frames
look identical on the
angiogram. |
Q: OK. You and others feel that intravascular
ultrasound is critical in proper stent placement, but how many
interventional cardiologists
in the U.S. are able to interpret IVUS images, how many use it,
and do you think that can increase?
Dr. Hodgson:
Well, that's a constant source of frustration. I don't think
there's an interventionalist
practicing today who isn't
aware of IVUS, and hasn’t at least heard of or seen it. I
would say that there are far fewer, maybe 20%, who actually feel
comfortable interpreting it.
I think the
bulk of the people are able to be trained, certainly have the
skill set to do it, but
for whatever reason haven’t.
This may change when somebody says, “Wait a second, I want
documentation that you've done a good job here.” But nobody's
even asking for a follow-up on outcomes; nobody asks what percentage
of your patients has restenosis.
Q: How could this change?
Dr. Hodgson:
I think we need to continue to work on educating people to the
ease of use of IVUS. A lot
of the things have been
done lately with automatic border detection. And training sessions
are important but they don't drive utilization. They help the people
who want to do it, but they don't really drive new people to utilize
it, not until individual hospitals or insurers start saying “we
would like to see 100% documentation at one year of your patient
follow up.”
Now there
are centers that do that. Duke’s got a great database,
Cleveland Clinic’s has a good database, Washington Hospital
Center has a good database, Columbia-Presbyterian has a good database.
We've been offering guaranteed angioplasties. We tell the insurers, “Listen,
we’ll guarantee your angioplasty. If anything happens in
the next year we'll do it for free.” Because we know we do
a good job, and we attend to the details. But until the insurers
are willing to either pay for a difference or require follow-up
information, it's not going to change.
Also IVUS
and FFR have to be a full member of the family. My folks set
it up on every case. The IVUS
and the FFR are turned on, patients'
names are input, they are ready to go on every case. We don't open
the disposables, but the machinery is ready to go. So you say “let's
do FFR” -- it’s fine, it's simple. You throw the wire
on the table and we're up and running. They prefer that. At 2:00am
they don't mind doing this, because they know that we're
gonna get the right answer and be done faster, and they also recognize
that
we're
doing the right thing for the patient. And actually all the nurses
and techs in their hearts, that's what they want. They want the
right thing for the patient.
(Continue
to Part Two)
This interview was conducted in February 2008
by Burt Cohen of Angioplasty.Org.
|