|
|
 |
Dr. Hodgson is an internationally
acclaimed cardiologist who, prior to founding Santé Cardiology,
was the Chief of Academic Cardiology at St. Joseph Hospital
and Medical Center in Phoenix. Previously a faculty member
at the Medical College of Virginia and Case Medical School
in Cleveland, he has devoted much of his career to training
the next generation of physicians. He has served in many
administrative positions and developed four Cardiology Departments.
Dr. Hodgson is a Past President of the SCAI and
a founding member of the SCCT.
He has published over 200 peer reviewed articles, 8 books
or
book
chapters,
holds
two
patents and
developed the TeachIVUS and TeachFFR online
simulation training tools.
Angioplasty recently sat down with Dr. Hodgson to talk about
intravascular technologies. This interview is posted in two
parts:
- Part One discusses intravascular
ultrasound (IVUS) and how it can increase the accuracy
of stent placement, and the role of IVUS in the era of
DES 2.0;
- Part
Two discusses Fractional Flow Reserve
(FFR) with some thoughts on training and recommendations
for patients.
|
|
 John
McB. Hodgson, MD
John
McB. Hodgson, MD
Santé Cardiology
Phoenix, Arizona |
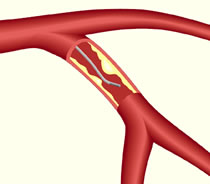
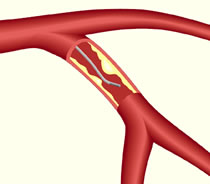
Q: You mentioned FFR, or Fractional
Flow Reserve, which measures any reduction in blood flow across a
section of the coronary artery. Can you explain how it’s done?
FloWire® Doppler
Guide Wire image, courtesy Volcano Corporation |
|
Dr. Hodgson:
FFR uses a guide wire with a pressure
sensor at the
tip.
We do 80% of ours through the diagnostic catheters, so you
don't even need a guiding catheter. It's actually very easy
to do; it takes one to two minutes, tops. We have it set up
on every case. We use, for the most part, intracoronary adenosine
as our hyperemic stimulus, although in rare cases we need to
use intravenous adenosine if there are multiple lesions or
ostial lesions.
The accuracy of the pressure measurement is fantastic.
We typically do three measures for a given lesion, with escalating
doses of adenosine, so that we're sure that we get maximal
hyperemia, and typically the values don't differ
by more than a hundredth, The other nice thing is there's
a
very small
gray zone which, for me, runs between about .75 and .81,
and in that area we use clinical judgment and other things
to decide
what to do. But it's unusual that a patient ends up in that
zone -- usually they're .9 or .6 so the answer's very easy. |
Q: How does measuring the reduced
blood flow affect the patient’s
treatment?
Dr. Hodgson: You have to make a couple of decisions when
you go into the lab, and the most important one is understanding
when not to do something. You need to be sure, that if
you're going to do an interventional procedure, whether it's surgery
or stenting
or balloons, bare metal stents, whatever, you need to be sure that
the patient really needs it.
Not all lesions need a stent. And people
argue “Well, I
have to do something….” Well you are doing something.
You've made a diagnosis, presumably you're going to put that person
on anti-thrombotic agents, agents for their lipids, control their
blood pressure, encourage them to stop smoking, exercise, etc.
So, you are doing something, but it may not be a stent. It's extremely
clear, from both the nuclear data as well as all the FFR data,
that if you do not have ischemia from a lesion, then there is no
benefit to revascularizing it.
Probably the strongest data here is the DEFER
trial (Deferral
Versus Performance of PTCA in Patients Without Documented Ischemia)
where they took cases where, due to blockages seen on the angiogram,
the operator intended to put a stent in. If the FFR was abnormal,
or ischemic, below .75, they went ahead and stented all of those;
the ones that were above .75, they randomized, to go ahead and
implant stents in half and leave the other half medically treated.
Now at 5 year follow-up, the ones who were left to be medically
treated did better in every regard: fewer events, fewer revascularizations,
less angina, etc.
I feel there's a concept out there among many
operators, that every lesion needs a stent, that by
plaque-sealing, we're
going to keep it from causing a problem in the future. But the
data just does not support that, if the lesion is not ischemic.
And I think the COURAGE trial, again, that plays
into that. In my mind, there's just no justification in a stable
patient to stent
a non-ischemic lesion. We're not talking about acute M.I.s, we're
not talking about acute non-Q.M.I.s. We're talking about the run
of the mill patient who somehow gets a false positive nuclear stress
test, or somehow gets on the cath table, and they start stenting
lesions. And there's a lot of that that goes on, unfortunately.
So, step
number 1, make sure that the lesion's really ischemic. If there's
any suspicion, I think that FFR should be done in the lab, to be
sure that you're not stenting a lesion which doesn't need to be
done.
But I do think it's a mistake to tell patients, “Well,
we're not going to do anything”, or “You don't need
anything done”. I think the proper approach is to say “Listen.
You're very lucky at this point. This blockage is not causing any
issues that we need to do anything invasive with, and we're going
to treat it aggressively with medical therapy”. It just depends
on how you present it to the patient. You can tell them that they're
lucky, that they don't have to have a stent. It's a good thing.
Q: For those who want to learn, what are the training opportunities?
Dr. Hodgson:
The bulk of the training opportunities come through courses
and
dinners
and things that are set up by the manufacturers. I think
we've kind of gone past the phase where we offer specific
IVUS training
as part of the big interventional meetings. There are certainly
always IVUS sessions at ACC or SCAI or AHA -- TCT uses a
lot of IVUS. But they don’t do it as part of every case.
We go to the hospital, give a grand rounds or lecture or dinner
meeting or cath conference or something. The most effective ones
in my mind are ones where we stay and work in the lab with people
to help them get through the fear factor of doing it. Another
issue that's critically important is training the techs and nurses
to be facile at using it.
I run 6-8 courses a year; we bring in 20 people. Now we're doing
a lot more dinner meetings, going out to the sites, so we can
get more people there. |
|

Dr. Hodgson
lecturing about IVUS during a session at the annual
TCT meeting |
The truth is we've been struggling for 13 years,
ever since we started the program when Cordis was co-marketing
with Endosonics,
to find a method which gets these guys excited. IVUS for whatever
reason, just never caught on as being something that we have to
do. You know when Rotablator came on everybody wanted to be trained.
And when DVI came out everybody wanted to be trained. When FoxHollow
came out everyone wanted to try it. In the early days, and I mean
early '90s, there was a lot of interest in IVUS and a lot of people
wanted to know about it, but then their interest falls off when
they don't feel that it makes a big difference to them, and it's
an attitude issue at that point.
A lot of younger fellows who've trained at a
place that uses a lot of IVUS come out and can't imagine doing
without it. Other
fellows come out of training and their mentors were less interested
in IVUS, and they come out with no interest in it. So, it's difficult.
The
three things that we learned in the mid '90s were they didn't
believe it improved patient outcomes, and we did a host of trials
in the late '90s to prove that that wasn't true. Second thing
was
they felt it was too hard to interpret, and we've spent a lot
of time and energy improving the interpretation and automating
the
border detection and all that kind of stuff, making the systems
easier to use. And the third thing is they said it was, it took
too much time, it was too difficult to do mechanically. We've
got integrated systems now, we've got very easy to use catheters,
and
that's just not true.
Q: What about the online program,
Teach IVUS – which
is co-sponsored by Volcano Therapeutics and Boston Scientific?

|
|
Dr. Hodgson: I'm biased
since I wrote it. It's a useful tool, sure. The nice thing
about
Teach IVUS and the thing that we do in all of our Teach products
(you know we have Teach CTA and Teach FFR, as well) is that
we give immediate expert feedback. So we require you to draw
or mark or point to or label or do something interactive with
the images, then you get immediate visual feedback as to what
the right answer was, where the drawing should have been, where
the border really was. And then we ask questions, based on
your measurements: “What would you do now?” So we do some sort
of teaching.
It's not about clinical decision making in terms
of cases; it's about “can you interpret these images properly?” And
so I think people can do that, it's non-threatening, you can
do it in your spare time, there's nobody pressuring you. I
think if every tech were to work on that, and a lot of labs
use it that way, then they'd be much more comfortable doing
the border tracing and border correction stuff that they need
to do during a live case. |
Q: What are the implications for patients here? Is this something
they should know about and ask for?
Dr. Hodgson: I think so. I think for the
most part if you ask doctors, “If
you're having a heart attack, do you want angioplasty or thrombolysis?”,
they all say they want angioplasty. If you ask doctors, “you
need a stent in your proximal LAD, do you want them
to use
IVUS or not”, they'll all say yes. So they all know the answer.
The patients, the educated ones will ask about it. I think it's
something that should be talked about. We do have it on the
SCAI web site describes some of these other
ancillary tools. We've toyed with a direct patient advertising
campaign. But I'm not sure how to get the message out to patients,
because it really has to be targeted to people who are likely to
have procedures. This is not a drug they can take, or a new exercise
regimen. FFR and IVUS are only applicable during a cath. So you
have to find the people who are about to get a cath and somehow
educate them.
Q: Angioplasty.Org currently
gets 100,000 visits a month. We’d
like to think we’re helping.
Dr. Hodgson: That's fantastic!
You should certainly encourage the patients to discuss with their
doctors two key things:
- is
this blockage really causing a restriction of blood flow,
or lack of blood flow to the heart, or however you want to
phrase
it, and
if not, I would prefer to continue my medical therapy,
and
- If this blockage needs to have an intervention,
how are
you
going to ensure that the stent, or whatever the intervention
is, is going to be done optimally? Are you going to
use IVUS or FFR
or some other method to be sure that you've done a
good job mechanically?
And those are two questions that
every patient
ought to ask when
they go in. Are you sure I need this and what's
the data, what's the proof, and number two, are you sure you
did a good
job? How
are you documenting your job? If you get a “well
it looks okay to me”, that's not good enough.
For the latest news and information about imaging, visit Angioplasty.Org's Intravascular Ultrasound
Center.
(Return to Part One)
This interview was conducted in February 2008
by Burt Cohen of Angioplasty.Org.
|