Drug-Eluting Stents - Part I
|
 |
The following is Part I of a two-part article which includes:
(1) An introduction to drug-eluting stents (also known as "drug coated stents", "medicated stents", or "DES");
(2) A history of drug-eluting stents, covering the evolution and mechanisms of these devices.
For more in-depth information and late-breaking articles about drug-eluting stents, visit our Drug-Eluting Stent Center.

Part 1. Drug-Eluting Stent Basics
Most coronary angioplasty procedures (also called "Percutaneous Coronary Interventions" or PCIs) involve implanting a stent, a small metal scaffold-like device. The stent is mounted on a balloon and guided to a blockage in the coronary artery. The balloon is inflated, compressing the obstructive plaque and opening up the blockage. The balloon is then deflated and withdrawn, but the stent is left behind to support the artery and keep it open as it heals.
Video not loaded
Animation of a drug-eluting stent, mounted on a balloon
courtesy Medtronic, Inc. |
Drug-eluting stents are metal stents that have been coated with a pharmacologic agent (drug) that is known to suppress restenosis: the reblocking or closing up of an artery after angioplasty due to excess tissue growth inside or at the edge of the stent.
Restenosis has a number of causes; it is a very complex process and the solution to its prevention is equally complex. Traditional bare-metal stents have restenosis rates of up to 25%; current 2nd and 3rd generation drug-eluting stents have reduced that rate to single digits.

Artist's rendition of coated stent on balloon in artery |
There are three major components to a drug-eluting stent:
- The metal stent structure, also called the stent platform; this is usually made of surgical stainless steel or a cobalt-chromium alloy; these all contain nickel;
- The polymer which coats the metal stent -- this coating contains the drug and delivers (elutes) it to the arterial wall over a period of time;
- The drug itself, which suppresses the formation of excess tissue, sometimes called "scar" tissue.
Precision Placement is Key to Efficacy of Stents

Interventional procedure being performed in the catheterization lab |
|
One key to long-lasting success of a stent is optimal placement of the device within the artery. There are several important decisions made by the interventional cardiologist when choosing and placing a stent:
- Correct sizing of the stent length to match the length of the lesion, or blocked area;
- Correct sizing of the stent diameter to match the true diameter of the of the artery;
- Sufficient deployment of the stent, making sure that the stent, once placed at the optimum location in the blocked artery, is expanded fully against the arterial wall – under-expansion can result in small gaps between the stent and arterial wall which can lead to serious problems such as blood clots, stent thrombosis (ST) or restenosis.
|
Angiogram |
The sizing and the assessments of stent expansion have traditionally been made by viewing a real-time angiogram in the catheterization lab during the procedure. In recent years more advanced technologies have become available that greatly increase the cardiologists' ability to identify where stents will be most effective and, if indicated, to measure, place and expand them with optimal precision.
Fractional Flow Reserve (FFR)
Fractional Flow Reserve is a measurement, performed during a catheterization or angioplasty, that makes it possible for the interventional cardiologist to calculate blood flow across an area of a coronary artery that is narrowed by plaque. Sometimes what appears to be a significant blockage on the angiogram turns out in fact to have sufficient blood flow and doesn't need stenting. Conversely, an artery that might appear to have only a slight closure on the angiogram may be atypical and is actually causing painful constriction of blood flow. Directly measuring actual blood flow helps in making these determinations.
 Read more about Fractional Flow Reserve. Read more about Fractional Flow Reserve.
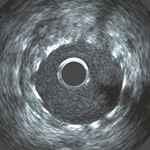
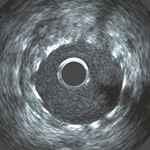
IVUS image of stent in artery |
Intravascular Ultrasound (IVUS)
Intravascular Ultrasound is an advanced imaging technique that, unlike traditional angiography, provides a cross-sectional picture of the artery from the inside out. Like fractional flow reserve, IVUS is performed during a procedure in the catheterization laboratory.
IVUS imaging can help doctors more accurately determine what size balloons and stents to use, and see whether they have achieved complete coverage of the diseased area and a complete expansion of the stent. Because ultrasound waves can penetrate beyond the surface of the arterial wall, it is relatively easy to see where the actual artery border is, beyond the accumulated plaque.
 Read more about Intravascular Ultrasound. Read more about Intravascular Ultrasound.
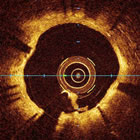
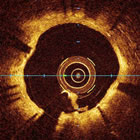
OCT image of stent in artery |
Optical Coherence Tomography (OCT)
OCT is a very new imaging technology that uses an optical laser to provide an image of the inside of the coronary artery. Although similar to intravascular ultrasound, Optical Coherence Tomography provides a much higher resolution image, high enough to look at the individual struts of the stent and to see if they have been covered by cells or not. OCT can also very accurately measure stent length, although it does not have the penetration into the arterial wall that IVUS has, so it has limitations in terms of assessing the true diameter of the native artery.
 Read more about Optical Coherence Tomography. Read more about Optical Coherence Tomography.
Correct Medication After Stenting is Key to Preventing Thrombosis (Blood Clots)
After receiving a drug-eluting stent, in addition to aspirin, the patient must take an second anti-clotting or antiplatelet drug, such as clopidogrel (Plavix), prasugrel (Effient), ticagrelor (Brilinta) or ticlopidine (Ticlid). This Dual Antiplatelet therapy (DAPT) needs to be continued for a year or more after the stenting in order to prevent the blood from reacting to the new device by thickening and clotting, thereby blocking the newly expanded artery (called stent thrombosis).
Ideally a smooth, thin layer of endothelial cells (the inner lining of the blood vessel) will grow over the stent during this period and the device will be incorporated into the arterial wall, reducing the tendency for clotting. Taking antiplatelet medication is crucial, since stent thrombosis is a rare but potentially catastrophic complication, usually resulting in heart attack or death.
Research is on-going as to the optimal length of time to continue antiplatelet medication, since these medications can be costly and have side effects. Hopefully we will soon have more precise ways of determining how long an individual should continue antiplatelet medication after stenting.
 Read more about Antiplatelet Therapy Read more about Antiplatelet Therapy
Continue to Part II. A History:
Evolution, Development and Outlook for Drug-Eluting Stents
Revised February 2013, Angioplasty.Org staff
|