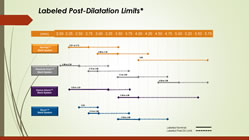
For the interventionalist, proper sizing of coronary stents is critical. While imaging via angiography has been the standard for years, newer intravascular imaging technologies, such as IVUS and OCT, are becoming more widely used, as evidence accrues that these modalities make a difference in outcomes. For example, IVUS (Intravascular Ultrasound) not only allows the measurement of the exact open diameter of the vessel, as seen on angiography, but it shows the “invisible to angiography” layer of plaque. plaque that will be compressed, so that a more accurate post-PCI diameter can be determined. Under-expanded stents have been associated with increased stent thrombosis and restenosis. Continue reading
Category Archives: Stent
Post-Dilatation Stent Sizes
Filed under Angiograms, Drug-Eluting Stents, Imaging, IVUS, OCT, Stent, Stent Thrombosis
History, Gruentzig, and Abbott’s Absorb “Dissolving Stent”

Abbott’s Absorb “Dissolving Stent”
There’s a lesson for the Absorb BVS in the history of interventional cardiology (an area of particular interest in this 40th anniversary of angioplasty year). There’s no question that the concept of a stent that dissolves and disappears is intriguing, and potentially clinically significant. Stents were invented because after balloon-only dilatation, the artery would sometimes collapse, or the spongy plaque would not compress neatly against the arterial wall, or the plaque would regrow, resulting in a very high rate of restenosis (reblocking of the artery).
Stents prevented all of this. Stents reduced the 3-5% acute closure rate that sent patients to bypass surgery after balloon angioplasty almost to zero. Continue reading
Filed under Bioresorbable Stents/Scaffolds, History, Stent
Status of the “Disappearing Stent” in Europe: It’s Complicated!
 Last night news began circulating on Twitter that Abbott’s Absorb BVS (Bioresorbable Vascular Scaffold) was being withdrawn from the European market. This information was prompted by several physicians posting on Twitter a March 31 “Urgent Field Safety Notice/Physician Advisory” letter from Abbott addressed to “Valued Abbott Vascular Customer.”
Last night news began circulating on Twitter that Abbott’s Absorb BVS (Bioresorbable Vascular Scaffold) was being withdrawn from the European market. This information was prompted by several physicians posting on Twitter a March 31 “Urgent Field Safety Notice/Physician Advisory” letter from Abbott addressed to “Valued Abbott Vascular Customer.”
A number of news sources, including this one, posted articles and tweets to the effect that the Absorb was being taken off the commercial markets and, as the letter stated, “Effective May 31, 2017, the device will only be available in clinical register setting at select sites/institutions that will play a pivotal role in the monitoring of this technology until Summer 2018 at which time the situation will be reviewed.”
This morning Abbott reacted to this initial flurry of reports that they had “pulled the Absorb” with some clarification: specifically that the Absorb is NOT being pulled from the market and still retains the CE Mark. An Abbott spokesperson told Angioplasty.Org, “Absorb will continue to be commercially available in Europe through the registries.”
But the relationship, as they say on Facebook, is complicated.
Interventional Cardiology Late-Breakers at ACC.17

Washington Convention Center
Over the next three days, a voluminous amount of data will be presented, shared, and debated among an estimated 18,000 attendees of the annual meeting of the American College of Cardiology, this year held in Washington, DC.
While the meeting covers the whole spectrum of cardiology and heart-related issues, there are a number of studies and late breaking clinical trials specific to the subspecialty of interventional cardiology. Continue reading
iFR and iFR Scout to be Featured in Live Case from Hammersmith
Dr. Justin Davies discusses value of using physiology-guided PCI
If you’ve been wondering what iFR (Instant wave-Free Ratio) is, how it works, how it compares to FFR (Fractional Flow Reserve) and, most importantly, how it affects clinical outcomes, then click here to register for a free, online, interactive live case being done on Monday, April 13, 2:30pm-3:30pm London Time, 9:30am-10:30am New York Time).
Interactive: that means you can ask questions!
Dr. Justin E Davies, interventional cardiologist at Imperial College NHS Trust, and developer of iFR, will be performing and guiding the worldwide audience through a live complex PCI multivessel case, using physiology to guide his procedure. Continue reading

 At this week’s annual European Society of Cardiology Congress in Rome, an important randomized clinical trial on stents was presented by Professor Kaare H. Bønaa, MD, PhD of the Clinic for Heart Disease, St. Olav’s University Hospital in Trondheim, Norway. Called NORSTENT, short for the “Norwegian Coronary Stent Trial,” this was the largest stent trial ever conducted, with 9,013 patients followed for six years. That’s serious!
At this week’s annual European Society of Cardiology Congress in Rome, an important randomized clinical trial on stents was presented by Professor Kaare H. Bønaa, MD, PhD of the Clinic for Heart Disease, St. Olav’s University Hospital in Trondheim, Norway. Called NORSTENT, short for the “Norwegian Coronary Stent Trial,” this was the largest stent trial ever conducted, with 9,013 patients followed for six years. That’s serious!  This past week saw publication of an update to the 2007 COURAGE trial which compared optimal medical therapy (OMT) to stenting (PCI) as the initial management strategy for stable coronary artery disease. (Please note the phrase “initial management strategy.” This will not be the last time you see it in this post.)
This past week saw publication of an update to the 2007 COURAGE trial which compared optimal medical therapy (OMT) to stenting (PCI) as the initial management strategy for stable coronary artery disease. (Please note the phrase “initial management strategy.” This will not be the last time you see it in this post.)

